Early Orthopedic Class III Treatment with a Modified Tandem Appliance
Growing patients with dentofacial deformities characterized by either a midfacial deficiency or true mandibular prognathism are perhaps the most challenging cases for the clinician to manage. In patients with midfacial deficiency, the current clinical protocol calls for orthopedic maxillary protraction by means of elastics to either an extraoral facemask or a chin cup.1,2 A maxillary expander is often used to enhance the orthopedic effect.3,4
If the patient is motivated enough to wear a facemask, treatment is likely to be successful.5,6 Downward and forward movement of the maxilla, an increase in overjet,7-12 and a backward rotation of the mandible with increased anterior facial height have all been documented with facemask therapy.13-16
The major problem, however, has been one of compliance, due to both the physical appearance of the extraoral appliance and skin irritation from the anchorage pads. This article presents an intraoral appliance that has been used clinically to achieve successful results in such cases without relying on unusual patient cooperation.
Differential Diagnosis
Careful evaluation of the diagnostic records, in conjunction with the clinical examination and medical history, is critical. If the patient presents with an anterior crossbite, the clinician must distinguish between the dental component and the skeletal growth component. Furthermore, a skeletal development problem must be differentiated between mandibular prognathism and midfacial maxillary deficiency.
Similar articles from the archive:
The Modified Tandem Appliance* (MTA) shown in this article is designed for Class III patients with skeletal midfacial deficiencies.
Appliance Design
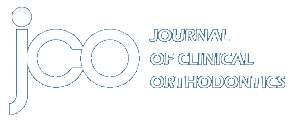
The MTA has three components, one fixed and two removable. The upper fixed appliance can be a traditional maxillary expander, with or without palatal acrylic (Fig. 1A), a QuadHelix**, or a Nance appliance. Soldered buccal arms are used for elastic traction. Upper brackets can be added, depending on the patient's age and clinical situation.
The lower appliance comprises a removable acrylic retainer with posterior occlusal coverage and buccal headgear tubes embedded in the area of the lower first molars (Fig. 1B). An .045" headgear facebow with the outer bows bent out for elastic attachment is inserted into the lower tubes.
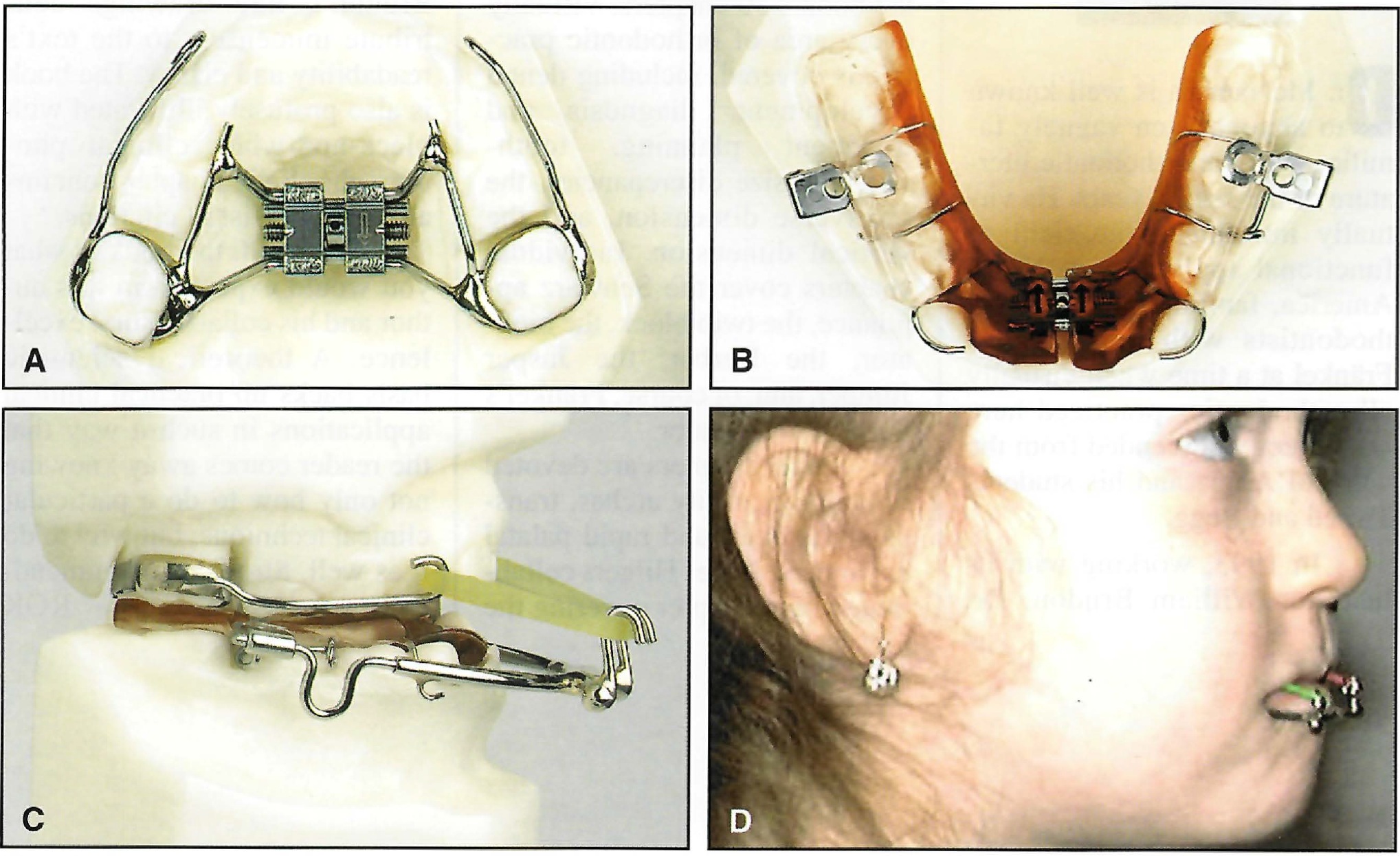
Fig. 1 A. Upper fixed appliance with palatal expander. B. Lower removable acrylic retainer with posterior occlusal coverage and buccal headgear tubes. C. Modified Tandem Appliance with heavy elastic traction from facebow to buccal arms of upper fixed appliance (photos © 2003 DynaFlex, Ltd.). D. Esthetic design promotes cooperation.
Delta clasps on the first permanent molars or second deciduous molars and "C" clasps on the lower deciduous canines are used for mechanical retention, which is essential for stability and cooperation. I recommend bonding small acrylic buttons to the labial surfaces of the lower canines so that the "C" clasps will snap over the buttons. In the deciduous dentition, where retention may be more of an issue, I have also added a lower midline expansion screw. I advise the parent to activate the screw one-quarter turn as necessary to ensure adequate retention between visits.
Heavy orthopedic elastic traction (400g per side) from the facebow to the buccal arms of the upper fixed appliance delivers the protraction force to the maxilla (Fig. 1C). However, patients are instructed to begin wearing the appliance with lighter 230g training elastics. I have found that the duration of wear is more significant than the force of the elastic. I request a minimum of 10-12 hours per day, including while sleeping. To my surprise, it is not unusual for patients to wear the MTA 14-16 hours per day, as esthetics and comfort do not seem to present problems (Fig.1D).
I see the patient one week later to verify compliance and check the appliance. On occasion, the buccal arms may irritate the inside of the cheeks, requiring minor adjustment. The patient is then scheduled every six weeks to monitor progress.
Case Report
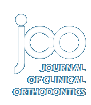
A female patient, age 3 years, 9 months, was initially referred by her pediatrician to an oral and maxillofacial surgeon. Clinical examination revealed a Class III malocclusion with a significant maxillary deficiency, an anterior crossbite, and a midfacial deficiency.
The patient's family had a history of thalassemia, but she had not been diagnosed with this condition. Her mother did relate that the patient had had multiple episodes of earache, with fluid behind the drums, and had difficulty breathing through her nose. The patient also demonstrated some lisping, and her mother confirmed that her articulation was affected.
It has been well documented that mouth-breathing as a result of nasopharyngeal blockage can have a significant effect on facial growth and development, causing maxillary retrusion and a downward and forward positioning of the mandible in an effort to open the airway.17,18 The patient was referred to an otolaryngologist with are commendation for a speech evaluation. Based on her age and level of maturity, she was placed on one-year recall.
A year later, initial orthodontic records were taken (Fig. 2). My original plan was to place an upper fixed expander and initiate maxillary protraction with a conventional facemask, but my previous results with facemask therapy had been mixed due to cooperation problems. After reading an article on a Tandem Appliance for orthopedic Class III correction that seemed much more patient-friendly than a facemask,19 I discussed the appliance with the patient's mother and obtained informed consent.
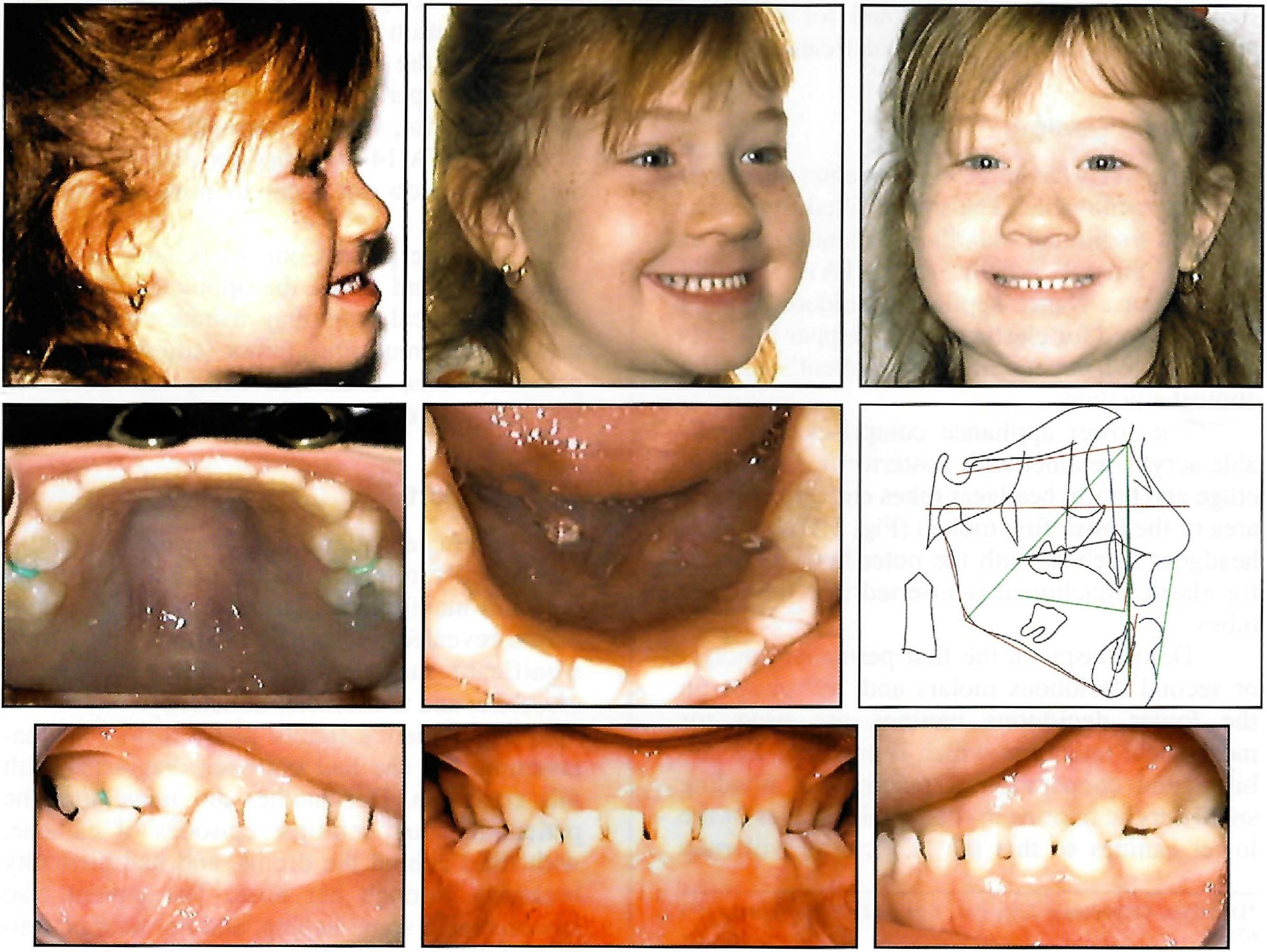
Fig. 2 4-year-old female patient with anterior crossbite and midfacial deficiency before treatment.
Instead of using two removable appliances, I modified the design to include a fixed maxillary component. The upper appliance had both palatal and labial bows for stability and soldered buccal arms for elastic attachment. In subsequent cases, I have used fixed expanders and transpalatal arches with equal effectiveness. A recent study has shown no significant orthopedic benefit from palatal expansion prior to facemask therapy.20
After the upper second deciduous molars were banded, we took upper and lower impressions and sent them with a wax bite registration to the laboratory for fabrication of an MTA appliance. Upon delivery, an 8oz, 230g training elastic (Panther***) was used for six weeks, followed by a 14oz, 400g elastic (Walrus***).
The patient was seen at six-week intervals for 12 months. The upper fixed appliance was then removed at the request of the otolaryngologist for removal of the tonsils and adenoids. After surgery, the appliance was recemented; the upper permanent incisors erupted favorably three months later. The MTA was removed after another four months (Fig. 3).
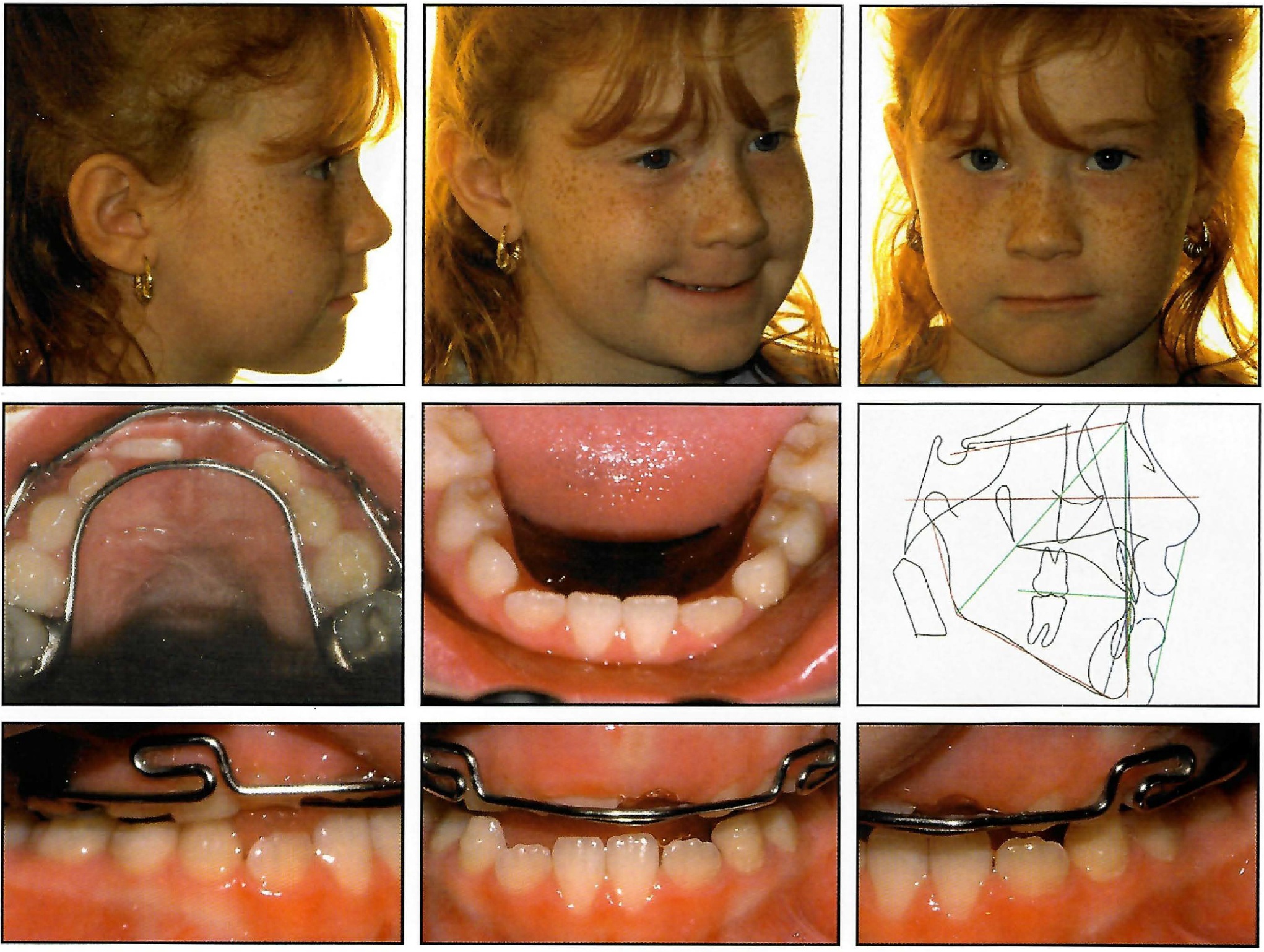
Fig. 3 Patient prior to removal of MTA, after 19 months of treatment.
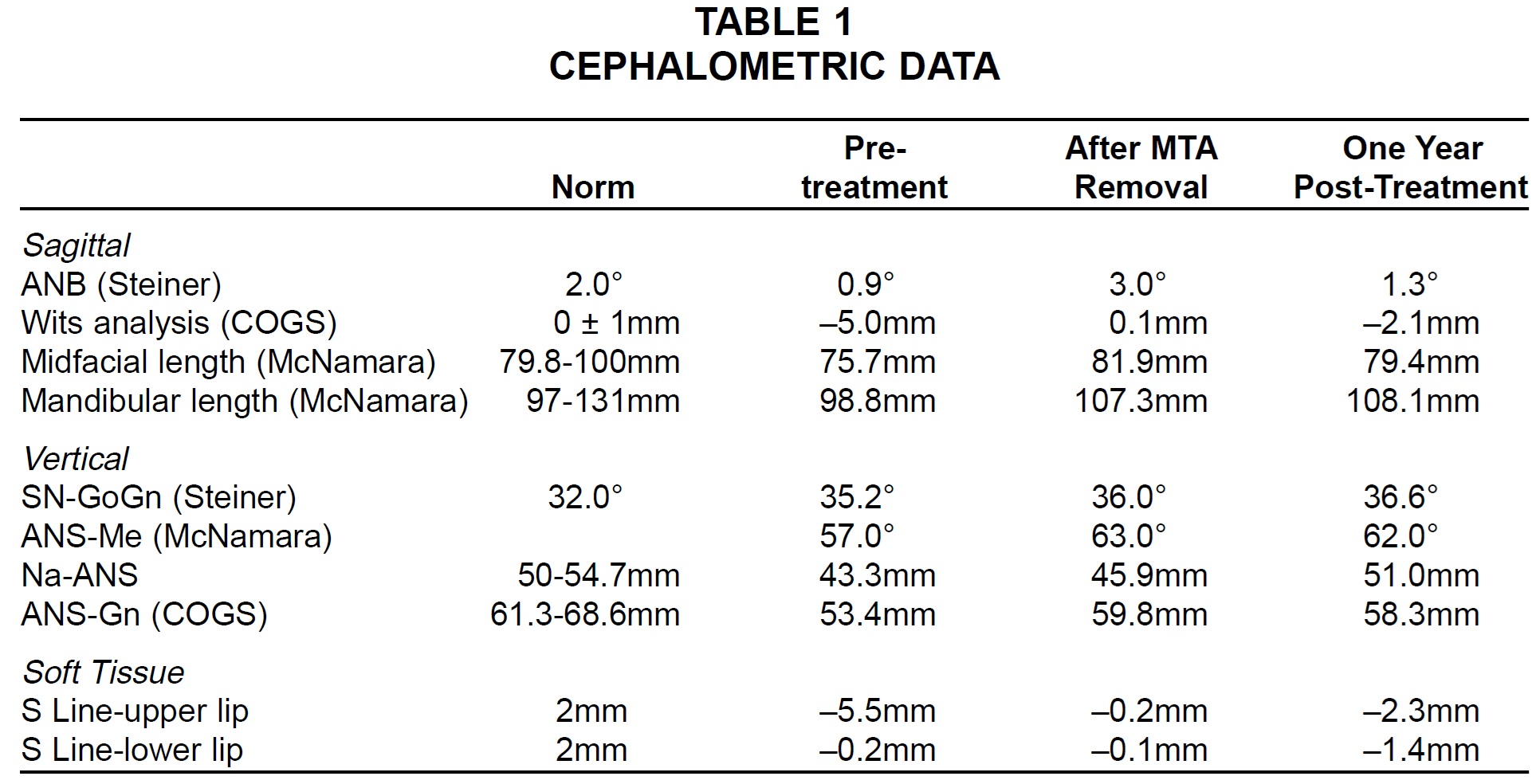
Cephalometric evaluation revealed a significant skeletal improvement, an increased vertical dimension, and a substantial improvement in facial balance (Table 1).
No retention appliances were used. A year or more after treatment, the patient has shown a stable Class I occlusion with good facial esthetics (Fig. 4). The relapse tendency toward a skeletal Class III pattern (Fig. 5) would be expected and has not been clinically significant.
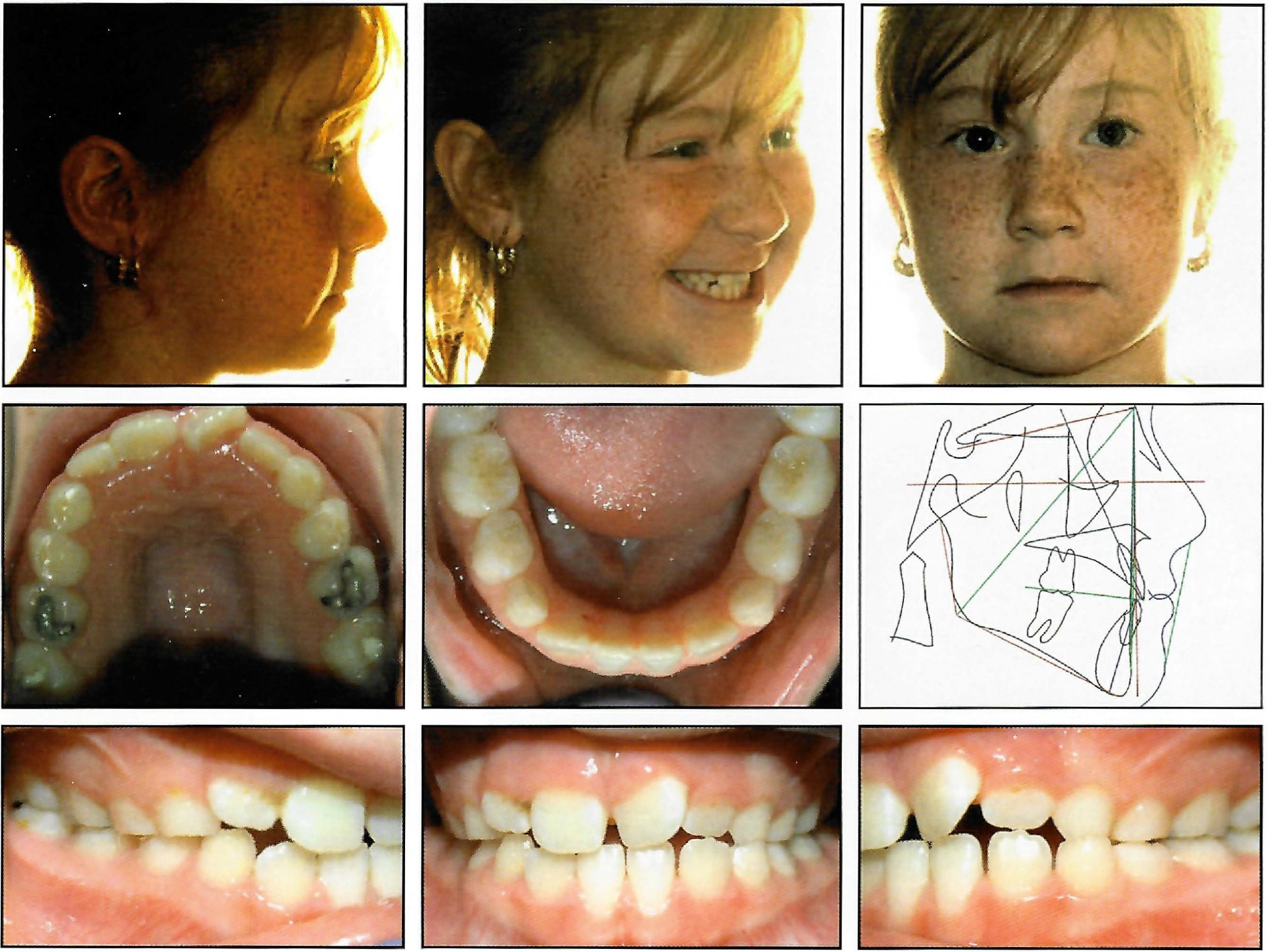
Fig. 4 Patient one year after treatment (cephalometric tracing) and 18 months after treatment (photographs).
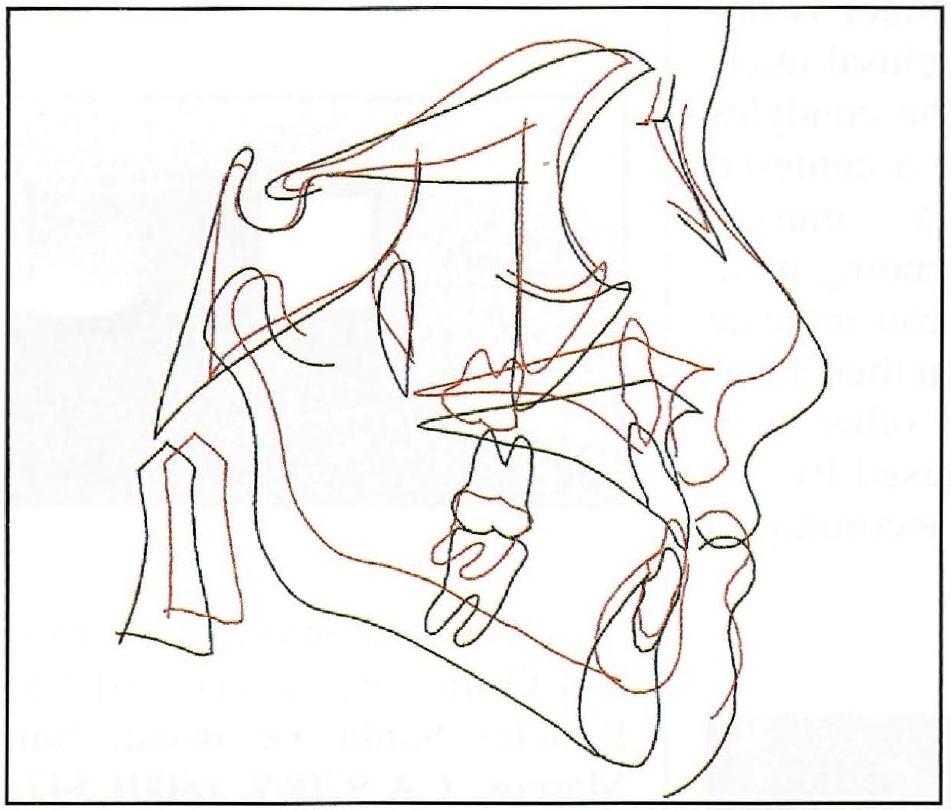
Fig. 5 Superimposition of cephalometric tracings before treatment (red) and one year after treatment (black).
Conclusion
I have found the Modified Tandem Appliance to be an effective tool in treating developing Class III malocclusions with skeletal maxillary deficiencies and deep anterior overbites.21 The action of the appliance is the same as with conventional facemask therapy, but with much better cooperation and fewer adjustments. Patients have not experienced any TMJ discomfort or pain despite the heavy elastic forces.
FOOTNOTES
- *DynaFlex Orthodontic Lab, P.O. Box 142399, St. Louis, MO 63114.
- **RMO, Inc., P.O. Box 17085, Denver, CO 80217.
- ***Ormco/“A” Company, 1717 W. Collins Ave., Orange, CA 92867.
REFERENCES
- 1. Turley, P.K.: Orthopedic correction of Class III malocclusion with palatal expansion and custom protraction headgear, J. Clin. Orthod. 22:314-325, 1988.
- 2. Hideo, M.: Early application of chincup therapy to skeletal Class III malocclusion, Am. J. Orthod. 121:584-585, 2002.
- 3. Alcan, T.; Keles, A.; and Erverdi, N.: The effects of a modified protraction headgear on maxilla, Am. J. Orthod. 117:27-38, 2000.
- 4. Ngan, P.; Hagg, U.; Yiu, C.; Merwin, D.; and Wei, S.H.: Soft tissue and dentoskeletal profile changes associated with maxillary expansion and protraction headgear treatment, Am. J. Orthod. 109:38-49, 1996.
- 5. Suda, N.; Ishii-Suzuki, M.; Hirose, K.; Hiyama, S.; Suzuki, S.; and Kuroda, T.: Effective treatment plan for maxillary protraction: Is the bone age useful to determine the treatment plan? Am. J. Orthod. 118:56-62, 2000.
- 6. Saadia, M. and Torres, E.: Vertical changes in Class III patients after maxillary protraction with expansion in the primary and mixed dentition, Pediat. Dent. 23:125-130, 2001.
- 7. Jager, A.; Braumann, B.; Kim, C.; and Wahner, S.: Skeletal and dental effects of maxillary protraction in patients with Angle Class III malocclusion. A meta-analysis, J. Orofac. Orthop. 62:275-84, 2000.
- 8. Sung, S.J. and Baik, H.S.: Assessment of skeletal and dental changes by maxillary protraction, Am. J. Orthod. 114:492-502, 1998.
- 9. Shanker, S.; Ngan, P.; Wade, D.; Beck, M.; Yiu, C.; Hagg, U.; and Wei, S.H.: Cephalometric A point changes during and after maxillary protraction and expansion, Am. J. Orthod. 110:423-430, 1996.
- 10. Chong, Y.H.; Ive, J.C.; and Artun, J.: Changes following the use of protraction headgear for early correction of Class III malocclusion, Angle Orthod. 66:351-362, 1996.
- 11. Ngan, P.; Wei, S.H.; Hagg, U.; Yiu, C.K.; Merwin, D.; and Stickel, B.: Effect of protraction headgear on Class III malocclusion, Quintess. Int. 23:197-207, 1992.
- 12. Mermigos, J.; Full, C.A.; and Andreasen, G.: Protraction of the maxillofacial complex, Am. J. Orthod. 98:47-55, 1990.
- 13. Kajiyama, K.; Murakami, T.; and Suzuki, A.: Evaluation of the modified maxillary protractor applied to Class III malocclusion with retruded maxilla in early dentition, Am. J. Orthod. 118:549-559, 2000.
- 14. Takada, K.; Petdachai, S.; and Sakuda, M.: Changes in dentofacial morphology in skeletal Class III children treated by a modified maxillary protraction headgear and a chin cup: A longitudinal cephalometric appraisal, Eur. J. Orthod. 15:211-221, 1993.
- 15. Ngan, P.: Biomechanics of maxillary expansion and protraction in Class III patients, Am. J. Orthod. 121:582-583, 2002.
- 16. Tindlund, R.S.: Skeletal response to maxillary protraction in patients with cleft lip and palate before age 10 years, Cleft Palate Craniofac. J. 31:295-308, 1994.
- 17. Subtelny, D.J.: Oral respiration: Facial maldevelopment and corrective dentofacial orthopedics, Angle Orthod. 50:147-164, 1980.
- 18. McNamara, J.A.: Influences of respiratory pattern on craniofacial growth, Angle Orthod. 51:269-300, 1981.
- 19. Chun, Y.S.; Jeong, S.G.; Row, J.; and Yang, S.J.: A new appliance for orthopedic correction of Class III malocclusion, J. Clin. Orthod. 32:705-711, 1999.
- 20. . Turley, P.: Managing the developing Class III malocclusion with palatal expansion and faskmask therapy, Am. J. Orthod. 122:349-352, 2002.
- 21. Pangrazio-Kulbersh, V.; Berger, J.; and Kersten, G.: Effects of protraction mechanics on the midface, Am. J. Orthod. 114:484-491, 1998.